 On Wednesday July 26th, BBC showed a thoughtful, well-researched Panorama documentary called A Prescription for Murder?. The programme was directed and introduced by Shelley Jofre (left), who, several years ago, exposed The Secrets of Seroxat.
On Wednesday July 26th, BBC showed a thoughtful, well-researched Panorama documentary called A Prescription for Murder?. The programme was directed and introduced by Shelley Jofre (left), who, several years ago, exposed The Secrets of Seroxat.
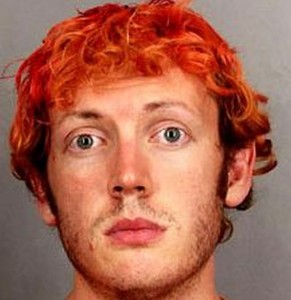 Most of the recent documentary was devoted to the so-called “Batman killer” James Holmes (right), a neuroscience graduate who shot dead 12 people and injured 70 in a Colorado cinema in 2012. He had been taking the SSRI antidepressant Sertraline (Zoloft), along with Clonazepam, a benzodiazepine.
Most of the recent documentary was devoted to the so-called “Batman killer” James Holmes (right), a neuroscience graduate who shot dead 12 people and injured 70 in a Colorado cinema in 2012. He had been taking the SSRI antidepressant Sertraline (Zoloft), along with Clonazepam, a benzodiazepine.
 In the run-up to the programme, two significant interviews were published. In the Sunday Times on July 23rd, Katinka Blackford Newman (left) was interviewed by Oliver Thring.
In the run-up to the programme, two significant interviews were published. In the Sunday Times on July 23rd, Katinka Blackford Newman (left) was interviewed by Oliver Thring.
Katinka, who was one of the principal researchers on the Panorama documentary, was the author of The Pill That Steals Lives. At its launch a year ago, I was privileged to have met David Carmichael, who had travelled from Canada.
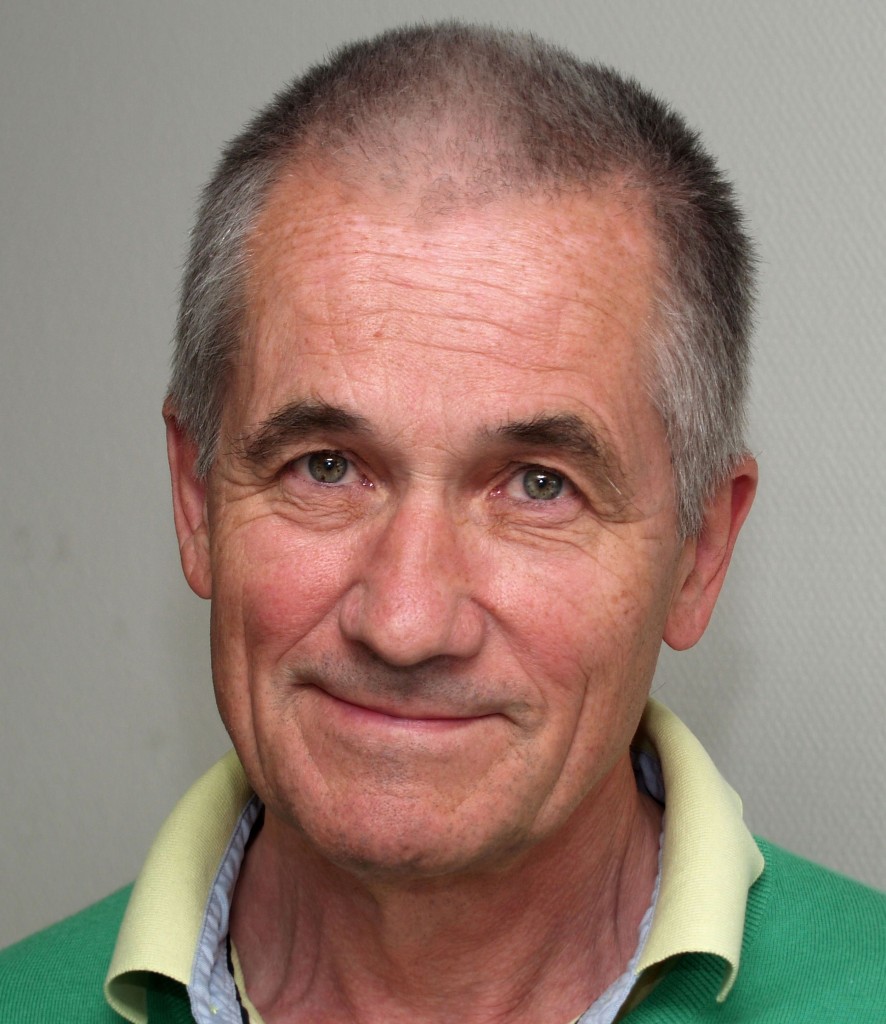
 In 2004 David (right), who had never shown any symptoms of psychosis before being prescribed Seroxat, strangled his 11-year-old son Ian. He was judged to be “not criminally responsible on account of a mental disorder” for murdering his son and, in 2009, he received an absolute discharge. Caroline Scott’s interview with David was published in the Daily Mail on the day before the documentary was shown.
In 2004 David (right), who had never shown any symptoms of psychosis before being prescribed Seroxat, strangled his 11-year-old son Ian. He was judged to be “not criminally responsible on account of a mental disorder” for murdering his son and, in 2009, he received an absolute discharge. Caroline Scott’s interview with David was published in the Daily Mail on the day before the documentary was shown.
 Another guest at the launch of Katinka’s book was Leonie Fennell, who had travelled from Ireland. In 2009, Leonie’s son, 22-year-old student Shane Clancy (left) fatally stabbed his ex-girlfriend’s new boyfriend, injured two others, then died after stabbing himself 19 times. Shane had no history whatsoever of violence, self-harm or mental instability of any sort. However, a few weeks before the tragedy, Shane had gone to see a doctor as he was feeling low after breaking up with his girlfriend, and was prescribed the antidepressant Citalopram (Celexa). At Shane’s inquest, the jury decided that Citalopram had probably caused Shane’s death and thus rejected a suicide verdict.
Another guest at the launch of Katinka’s book was Leonie Fennell, who had travelled from Ireland. In 2009, Leonie’s son, 22-year-old student Shane Clancy (left) fatally stabbed his ex-girlfriend’s new boyfriend, injured two others, then died after stabbing himself 19 times. Shane had no history whatsoever of violence, self-harm or mental instability of any sort. However, a few weeks before the tragedy, Shane had gone to see a doctor as he was feeling low after breaking up with his girlfriend, and was prescribed the antidepressant Citalopram (Celexa). At Shane’s inquest, the jury decided that Citalopram had probably caused Shane’s death and thus rejected a suicide verdict.
Although most of the Panorama documentary was devoted to James Holmes, both David and Leonie appeared in short interviews with Shelley Jofre. It is interesting to note at this point that, in Canada and Ireland, juries decided that, in these two instances at least, there was a causal link between antidepressants and homicide. This is something which is continually denied by pharmaceutical companies and their acolytes.
 Before the documentary had even been shown, the Science Media Centre orchestrated a campaign of mis-information and denigration against the programme. Among the psychiatrists enlisted to provide “expert comments” were Allan Young (right) and Carmine Pariante, both of whom have financial links to pharmaceutical companies that make antidepressants. Moreover, the two professors are employed by Kings College, London, which recently welcomed the UK managing director of Pfizer (makers of Sertraline) on to its board.
Before the documentary had even been shown, the Science Media Centre orchestrated a campaign of mis-information and denigration against the programme. Among the psychiatrists enlisted to provide “expert comments” were Allan Young (right) and Carmine Pariante, both of whom have financial links to pharmaceutical companies that make antidepressants. Moreover, the two professors are employed by Kings College, London, which recently welcomed the UK managing director of Pfizer (makers of Sertraline) on to its board.
 Another contributor was Wendy Burn (left), the new president of the Royal College of Psychiatrists, who also wrote an article for The Times, written before the broadcast but published the morning after it, entitled “Stop this dangerous scaremongering over antidepressants”.
Another contributor was Wendy Burn (left), the new president of the Royal College of Psychiatrists, who also wrote an article for The Times, written before the broadcast but published the morning after it, entitled “Stop this dangerous scaremongering over antidepressants”.
There was little criticism of the programme after it had actually been shown.
 But then, on Twitter, the Royal College of Psychiatrists (@rcpsych) announced that Wendy Burn and Carmine Pariante would be holding an hour-long Q and A session on August 3rd, using the hashtag #ADsMythBuster (right). It seemed as if the college’s intention was to use Twitter to “bust” what they regarded as “myths” surrounding antidepressants.
But then, on Twitter, the Royal College of Psychiatrists (@rcpsych) announced that Wendy Burn and Carmine Pariante would be holding an hour-long Q and A session on August 3rd, using the hashtag #ADsMythBuster (right). It seemed as if the college’s intention was to use Twitter to “bust” what they regarded as “myths” surrounding antidepressants.
The questions started to come in well before the session, but no replies were tweeted before the appointed hour.
It wasn’t long before the first myth was busted by Wendy and Carmine. The surprise was that this particular myth had been perpetrated for many years by their colleagues, as well as other prescribers: “The old idea that ADs correct a chemical imbalance in the brain is an over-simplification and we do not support this view.”
I felt optimistic, and asked, to no avail: “Now that you’ve busted the “chemical imbalance” myth, are you going to bust the “no causal link with violence” myth next?”
Alas, it was not to be. This was the nearest we would get to a proper myth buster during the hour. Before long, the assertion that “ADs do have measurable biological effects; increasing new brain cells & reducing stress hormones” produced a number of retorts, both serious and light-hearted, from those who found this quite difficult to believe.
Asked about withdrawal, the reply was: “Not everyone gets withdrawal symptoms. You must come off ADs slowly over 8-12 weeks with support of your doctor.” This response was queried by a participant, who was told: “Everyone is different & you need to plan this with your doctor. Most people are okay with 8-12 weeks to reduce and stop”.
Somebody asked about the best ADs for a mother to use before and after birth and was told: “Preferred choice are SSRIs esp Fluoxetine in pregnancy & Sertraline in breastfeeding”. The questioner was not told that the best option was to avoid antidepressants altogether during this period.
 When a question was asked about whether antidepressants can be used to treat bi-polar, the reply was “Yes they can, but preferably with a mood stabiliser”. Aine O’Beirne (left) was quick to retort: “You say use SSRIs to treat Bipolar when SSRIs are one of the causes of Bipolar epidemic”.
When a question was asked about whether antidepressants can be used to treat bi-polar, the reply was “Yes they can, but preferably with a mood stabiliser”. Aine O’Beirne (left) was quick to retort: “You say use SSRIs to treat Bipolar when SSRIs are one of the causes of Bipolar epidemic”.
To a question about side-effects causing sexual problems, the reply was: “Yes they are common with SSRIs, usually improves but if not discuss with your doctor”.
And when they were asked about the length of treatment, the professors answered: “Patients are taking ADs for longer according to the correct guidelines for treatment & this is a good thing”.
The reply to a question about the record high numbers of antidepressants prescribed was: “We believe it’s because more people are coming forward & reduced stigma – this is a good thing”.
The person who asked about the benefits of taking antidepressants was told: “Sadness improves within days, new studies show that improvement is faster than we originally thought – within weeks”.
And to the person whose antidepressants weren’t working, the answer was: “There are recommended combinations of ADs & other meds for patients who don’t respond”.
 To a question about the link with violence, Wendy and Carmime (right) stuck with the ridiculous line: “In adults there is no evidence ADs increase hostility & aggressiveness”. This prompted my question: “Did you actually watch “Panorama” last week?”
To a question about the link with violence, Wendy and Carmime (right) stuck with the ridiculous line: “In adults there is no evidence ADs increase hostility & aggressiveness”. This prompted my question: “Did you actually watch “Panorama” last week?”
I asked several questions, and received replies to two of them. The first, about sanctioning members for not following NICE Guidelines, elicited the response: “The guidelines are guidelines not the law, we encourage people to follow them”.
In the other, I asked “Is it acceptable to compel somebody to take ADs in order to be given sickness benefit?”. The reply, “Nobody should be forced to have any treatment to be given sickness benefit”, gave me encouragement, although this message needs to be passed on to the guilty GPs.
It was obvious that only a small proportion of questions could be answered, but I had a feeling that the more difficult ones were avoided in favour of those for which pre-prepared replies were available.
 One of the most frustrated participants was Lucy Johnstone (left), who submitted the three questions that had the most re-tweets, but never received an answer to any of them. Eventually, to the question “Why are rocketing prescribing levels not reducing rates of depression and suicide, if the drugs are effective?”, Lucy commented: “71 retweets & 88 likes. Deserves an answer”.
One of the most frustrated participants was Lucy Johnstone (left), who submitted the three questions that had the most re-tweets, but never received an answer to any of them. Eventually, to the question “Why are rocketing prescribing levels not reducing rates of depression and suicide, if the drugs are effective?”, Lucy commented: “71 retweets & 88 likes. Deserves an answer”.
A complete list of questions and answers has been compiled by James Moore, while Aine has published a selection on Storify.
 The following day, the overriding impression was that if the College saw their “MythBuster” session as a PR exercise, then they had failed. The reaction of Fiona French (right), writing in the BMJ, was typical: “The online support community submitted many, many intelligent and probing questions. The responses were few in number and lacking in substance. We were advised that the Royal College ‘thinks’ the benefits of antidepressants outweigh the harms but no supporting evidence was provided.”
The following day, the overriding impression was that if the College saw their “MythBuster” session as a PR exercise, then they had failed. The reaction of Fiona French (right), writing in the BMJ, was typical: “The online support community submitted many, many intelligent and probing questions. The responses were few in number and lacking in substance. We were advised that the Royal College ‘thinks’ the benefits of antidepressants outweigh the harms but no supporting evidence was provided.”
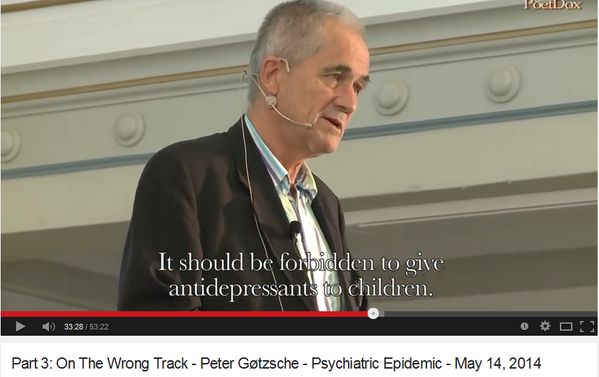
My final contribution was to suggest that: “Next time @rcpsych need an #ADsMythBuster, they should call @PGtzsche1.”
I was, in fact, referring to Professor Peter Gøtzsche (top), one of the world’s most knowledgeable and influential professors in this field. In September 2015, I attended a conference in Copenhagen which Peter had organised. The theme of the event was Psychiatric drugs do more harm than good. I wouldn’t have expected the Pharma-influenced Royal College of Psychiatrists to agree, but the arguments were compelling.
 In January 2014, Dr David Healy (left) published an article on his website which Peter had written, and in which he blew apart 10 myths that GSK, Lundbeck, Eli Lilly, Pfizer, etc would like us to believe. Here is Peter’s article:
In January 2014, Dr David Healy (left) published an article on his website which Peter had written, and in which he blew apart 10 myths that GSK, Lundbeck, Eli Lilly, Pfizer, etc would like us to believe. Here is Peter’s article:
At the Nordic Cochrane Centre, we have researched antidepressants for several years and I have long wondered why leading professors of psychiatry base their practice on a number of erroneous myths. These myths are harmful to patients. Many psychiatrists are well aware that the myths do not hold and have told me so, but they don’t dare deviate from the official positions because of career concerns.
Being a specialist in internal medicine, I don’t risk ruining my career by incurring the professors’ wrath and I shall try here to come to the rescue of the many conscientious but oppressed psychiatrists and patients by listing the worst myths and explain why they are harmful.
Myth 1: Your disease is caused by a chemical imbalance in the brain
Most patients are told this but it is completely wrong. We have no idea about which interplay of psychosocial conditions, biochemical processes, receptors and neural pathways that lead to mental disorders and the theories that patients with depression lack serotonin and that patients with schizophrenia have too much dopamine have long been refuted. The truth is just the opposite. There is no chemical imbalance to begin with, but when treating mental illness with drugs, we create a chemical imbalance, an artificial condition that the brain tries to counteract.
This means that you get worse when you try to stop the medication. An alcoholic also gets worse when there is no more alcohol but this doesn’t mean that he lacked alcohol in the brain when he started drinking.
The vast majority of doctors harm their patients further by telling them that the withdrawal symptoms mean that they are still sick and still need the medication. In this way, the doctors turn people into chronic patients, including those who would have been fine even without any treatment at all. This is one of the main reasons that the number of patients with mental disorders is increasing, and that the number of patients who never come back into the labour market also increases. This is largely due to the drugs and not the disease.
Myth 2: It’s no problem to stop treatment with antidepressants
A Danish professor of psychiatry said this at a recent meeting for psychiatrists, just after I had explained that it was difficult for patients to quit. Fortunately, he was contradicted by two foreign professors also at the meeting. One of them had done a trial with patients suffering from panic disorder and agoraphobia and half of them found it difficult to stop even though they were slowly tapering off. It cannot be because the depression came back, as the patients were not depressed to begin with. The withdrawal symptoms are primarily due to the antidepressants and not the disease.
Myth 3: Psychotropic drugs for mental illness are like insulin for diabetes
Most patients with depression or schizophrenia have heard this falsehood over and over again, almost like a mantra, in TV, radio and newspapers. When you give insulin to a patient with diabetes, you give something the patient lacks, namely insulin. Since we’ve never been able to demonstrate that a patient with a mental disorder lacks something that people who are not sick don’t lack, it is wrong to use this analogy.
Patients with depression don’t lack serotonin, and there are actually drugs that work for depression although they lower serotonin. Moreover, in contrast to insulin, which just replaces what the patient is short of, and does nothing else, psychotropic drugs have a very wide range of effects throughout the body, many of which are harmful. So, also for this reason, the insulin analogy is extremely misleading.
Myth 4: Psychotropic drugs reduce the number of chronically ill patients
This is probably the worst myth of them all. US science journalist Robert Whitaker demonstrates convincingly in “Anatomy of an Epidemic” that the increasing use of drugs not only keeps patients stuck in the sick role, but also turns many problems that would have been transient into chronic diseases.
If there had been any truth in the insulin myth, we would have expected to see fewer patients who could not fend for themselves. However, the reverse has happened. The clearest evidence of this is also the most tragic, namely the fate of our children after we started treating them with drugs. In the United States, psychiatrists collect more money from drug makers than doctors in any other specialty and those who take most money tend to prescribe antipsychotics to children most often. This raises a suspicion of corruption of the academic judgement.
The consequences are damning. In 1987, just before the newer antidepressants (SSRIs or happy pills) came on the market, very few children in the United States were mentally disabled. Twenty years later it was over 500,000, which represents a 35-fold increase. The number of disabled mentally ill has exploded in all Western countries. One of the worst consequences is that the treatment with ADHD medications and happy pills has created an entirely new disease in about 10% of those treated – namely bipolar disorder – which we previously called manic depressive illness.
Leading psychiatrist have claimed that it is “very rare” that patients on antidepressants become bipolar. That’s not true. The number of children with bipolar increased 35-fold in the United States, which is a serious development, as we use antipsychotic drugs for this disorder. Antipsychotic drugs are very dangerous and one of the main reasons why patients with schizophrenia live 20 years shorter than others. I have estimated in my book, ‘Deadly Medicine and Organized Crime’, that just one of the many preparations, Zyprexa (olanzapine), has killed 200,000 patients worldwide.
Myth 5: Happy pills* do not cause suicide in children and adolescents
Some professors are willing to admit that happy pills increase the incidence of suicidal behavior while denying that this necessarily leads to more suicides, although it is well documented that the two are closely related. Lundbeck’s CEO, Ulf Wiinberg, went even further in a radio programme in 2011 where he claimed that happy pills reduce the rate of suicide in children and adolescents. When the stunned reporter asked him why there then was a warning against this in the package inserts, he replied that he expected the leaflets would be changed by the authorities!
Suicides in healthy people, triggered by happy pills, have also been reported. The companies and the psychiatrists have consistently blamed the disease when patients commit suicide. It is true that depression increases the risk of suicide, but happy pills increase it even more, at least up to about age 40, according to a meta-analysis of 100,000 patients in randomized trials performed by the US Food and Drug Administration.
Myth 6: Happy pills have no side effects
At an international meeting on psychiatry in 2008, I criticized psychiatrists for wanting to screen many healthy people for depression. The recommended screening tests are so poor that one in three healthy people will be wrongly diagnosed as depressed. A professor replied that it didn’t matter that healthy people were treated as happy pills have no side effects!
Happy pills have many side effects. They remove both the top and the bottom of the emotions, which, according to some patients, feels like living under a cheese-dish cover. Patients care less about the consequences of their actions, lose empathy towards others, and can become very aggressive. In school shootings in the United States and elsewhere a striking number of people have been on antidepressants.
The companies tell us that only 5% get sexual problems with happy pills, but that’s not true. In a study designed to look at this problem, sexual disturbances developed in 59% of 1,022 patients who all had a normal sex life before they started an antidepressant. The symptoms include decreased libido, delayed or no orgasm or ejaculation, and erectile dysfunction, all at a high rate, and with a low tolerance among 40% of the patients. Happy pills should therefore not have been marketed for depression where the effect is rather small, but as pills that destroy your sex life.
Myth 7: Happy pills are not addictive
They surely are and it is no wonder because they are chemically related to and act like amphetamine. Happy pills are a kind of narcotic on prescription. The worst argument I have heard about the pills not causing dependency is that patients do not require higher doses. Shall we then also believe that cigarettes are not addictive? The vast majority of smokers consume the same number of cigarettes for years.
Myth 8: The prevalence of depression has increased a lot
A professor argued in a TV debate that the large consumption of happy pills wasn’t a problem because the incidence of depression had increased greatly in the last 50 years. I replied it was impossible to say much about this because the criteria for making the diagnosis had been lowered markedly during this period. If you wish to count elephants in Africa, you don’t lower the criteria for what constitutes an elephant and count all the wildebeest, too.
Myth 9: The main problem is not overtreatment, but undertreatment
Again, leading psychiatrists are completely out of touch with reality. In a 2007 survey, 51% of the 108 psychiatrists said that they used too much medicine and only 4 % said they used too little. In 2001–2003, 20% of the US population aged 18–54 years received treatment for emotional problems, and sales of happy pills are so high in Denmark that every one of us could be in treatment for 6 years of our lives. That is sick.
Myth 10: Antipsychotics prevent brain damage
Some professors say that schizophrenia causes brain damage and that it is therefore important to use antipsychotics. However, antipsychotics lead to shrinkage of the brain, and this effect is directly related to the dose and duration of the treatment. There is other good evidence to suggest that one should use antipsychotics as little as possible, as the patients then fare better in the long term. Indeed, one may completely avoid using antipsychotics in most patients with schizophrenia, which would significantly increase the chances that they will become healthy, and also increase life expectancy, as antipsychotics kill many patients.
How should we use psychotropic drugs?
I am not against using drugs, provided we know what we are doing and only use them in situations where they do more good than harm. Psychiatric drugs can be useful sometimes for some patients, especially in short-term treatment, in acute situations. But my studies in this area lead me to a very uncomfortable conclusion:
Our citizens would be far better off if we removed all the psychotropic drugs from the market, as doctors are unable to handle them. It is inescapable that their availability creates more harm than good. Psychiatrists should therefore do everything they can to treat as little as possible, in as short time as possible, or not at all, with psychotropic drugs.
At least Wendy Burn and Carmine Pariante admitted the first of Peter Gøtzsche’s myths. I look forward to a time when Myths 2-10 are dispelled by those who are at present prescribing a ridiculously high and ultimately harmful number of antidepressants.
* I am not comfortable with the phrase “happy pills”, but I have left the original text intact. It is probable that, in this context, the phrase is a literal translation of the Danish word “lykkepiller”.
Related Articles:
Mental Health Disability: the Antidepressant Connection
Suicide Prevention: a Conflict of Interest
Excellent blog, Brian – thank you – sharing widely …
Outstanding post on a great blog. Well done Brian.
It’s too dangerous to talk about these myths with any main stream psychiatrist – she/he will immediately label the patient as having no insight to his/her illness – and introduce more drugs. The worst thing is you see your loved one being harmed by these drugs and can’t speak your mind openly, fearing more bullying.
An essential and timely article, and I totally agree with the comments above.
I have referred the article / website to the Health Minister’s office as a ten-minute substitute for “The Sedated Society” book I sent to Jeremy Hunt, which he may find too lengthy to read.
With luck NICE, too, will get the message that SSRIs at least should be banned for doing more harm than good.
Impressive. Happy to have found this and will be sharing and supporting widely. In solidarity and gratitude for your work.